Designing Smarter Tools for Smarter Care
A role-sensitive dashboard and AI assistant built for VA clinicians navigating complex care.
BRIEF OVERVIEW
Virtual Care Manager (VCM) is the VA’s digital platform for enabling remote, patient-centered care, supporting everything from primary care and chronic disease management to mental health and specialty-specific workflows.
From December 2024 to May 2025, I led the design of VCM’s first integrated clinician dashboard and SARA, a GenAI-powered assistant. My role was to translate scattered clinical workflows into a modular, role-sensitive workspace where providers could finally see what mattered most at a glance.
Before this, VCM lacked a central, intelligent workspace for clinicians to monitor patients, surface high-priority issues, and respond in real time. Providers juggled multiple disconnected systems, leaving critical trends hidden in the noise.
I partnered with VA clinicians, AI engineers, and UX researchers to design a modular, role-aware dashboard and define SARA’s capabilities.
THE PROBLEM
Through early-stage research with 25 VA providers across primary care, specialty care, and mental health, we uncovered a recurring theme:
Providers were drowning in fragmented patient information spread across multiple EHR screens, lab portals, and messaging systems.
This led to:
Time Lost: “I spend 10–15 minutes per patient just hunting for the right data.” - Clinician
Missed Changes: “Subtle but important shifts, a blood pressure rise, a PHQ-9 bump, often slip through until it’s too late.” - Clinician
Protocol Drift: “Treatment cycles stall because no one realizes a step was missed.” - Clinician
Cognitive Strain: “Every visit feels like piecing together a puzzle from sticky notes, labs, and messages.” - Clinician
THE GOAL
Our goal was simple but ambitious: design a dashboard that does the heavy lifting for clinicians. A space that centralizes insights across domains, integrates SARA to surface what matters, and reduces chart-scanning time so providers can focus on care, not data hunting.
RESEARCH
Understanding the priorities and pain points of VA clinicians
Working closely with the VA’s human-centered design (HCD) team, I reviewed interview transcripts, observational data, and workflow analysis across specialties like mental health, primary care, and cardiology. Across the board, clinicians reported feeling overwhelmed by cluttered interfaces, disjointed tools, and a lack of role-specific views.
Across the board, clinicians reported feeling overwhelmed by cluttered interfaces, disjointed tools, and a lack of role-specific views.
“Every visit feels like starting from scratch. I have to hunt for what I need.”
We uncovered three major themes:
No clear starting point: Clinicians had no centralized view to prepare for a visit or assess next steps.
Role mismatch: Nurses, physicians, and specialists all received the same toolset, despite vastly different workflows.
Buried insights: Key information like protocol status, mood trends, or patient-submitted data often went unnoticed.
To illustrate this, we mapped the typical pre-visit workflow across five phases revealing just how fragmented and memory-reliant the process had become. Steps often involved switching between multiple tools, copy-pasting into Word, and using sticky notes to avoid losing track of tasks.
These findings shaped the foundation of our work:
We needed to create a dashboard that was focused, flexible, smart, and make room for SARA to surface what might otherwise be missed.
From Pain Points to Purposeful Design
We set out to reduce mental load, highlight what matters most, and give clinicians a grounded, actionable view of their day.
CONCEPT DEVELOPMENT
From Research to Concepts
I experimented with multiple wireframe variations, testing how different hierarchies shaped the experience: Information hierarchy: schedule-first, PGHD-first, or task-focused layouts.
Schedule-first views supported time management.
PGHD-first layouts emphasized remote monitoring.
Task-focused designs surfaced to-dos upfront.
Through feedback with clinicians, the winning direction was a modular grid, anchored by SARA’s proactive recommendations. This struck the balance between flexibility and focus.
The winning approach was a role-sensitive layout anchored by SARA’s recommendations, with flexible widgets for vitals, labs, care protocols, and specialty milestones. SARA’s conversational panel could surface at-risk patients, summarize charts, and draft outreach messages, while its design language showed transparency in “how” and “why” recommendations were made.
By aligning clinical priorities with AI opportunities, the concept evolved from a static dashboard to a living, adaptive workspace, one that could grow with the VA’s future AI initiatives.
FINAL DESIGNS
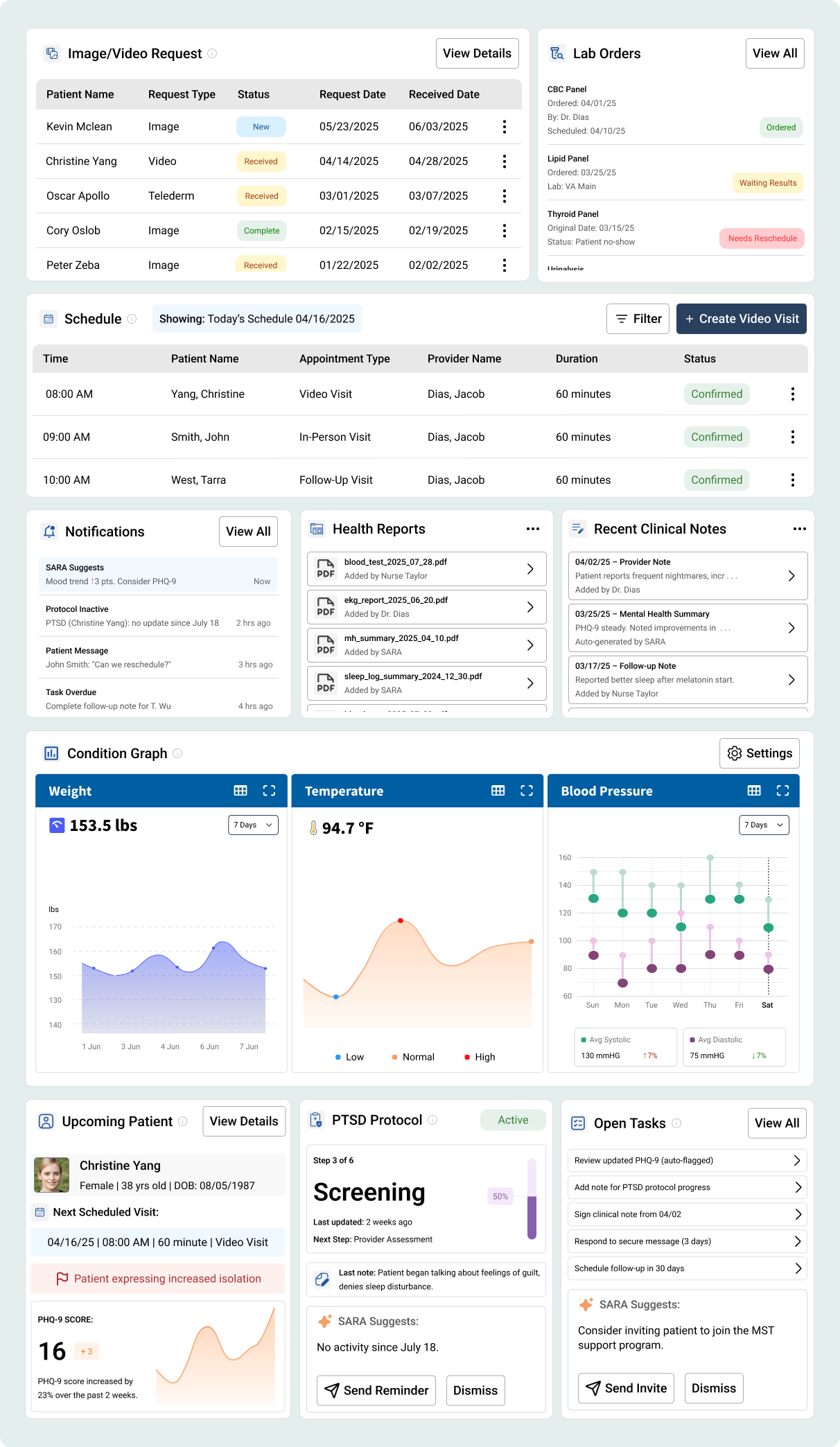
Widget System at a Glance
This isn’t just a dashboard. It’s a living workspace where clinicians can configure widgets for their practice, from cardiology vitals to oncology protocols, while SARA ensures nothing critical slips through.
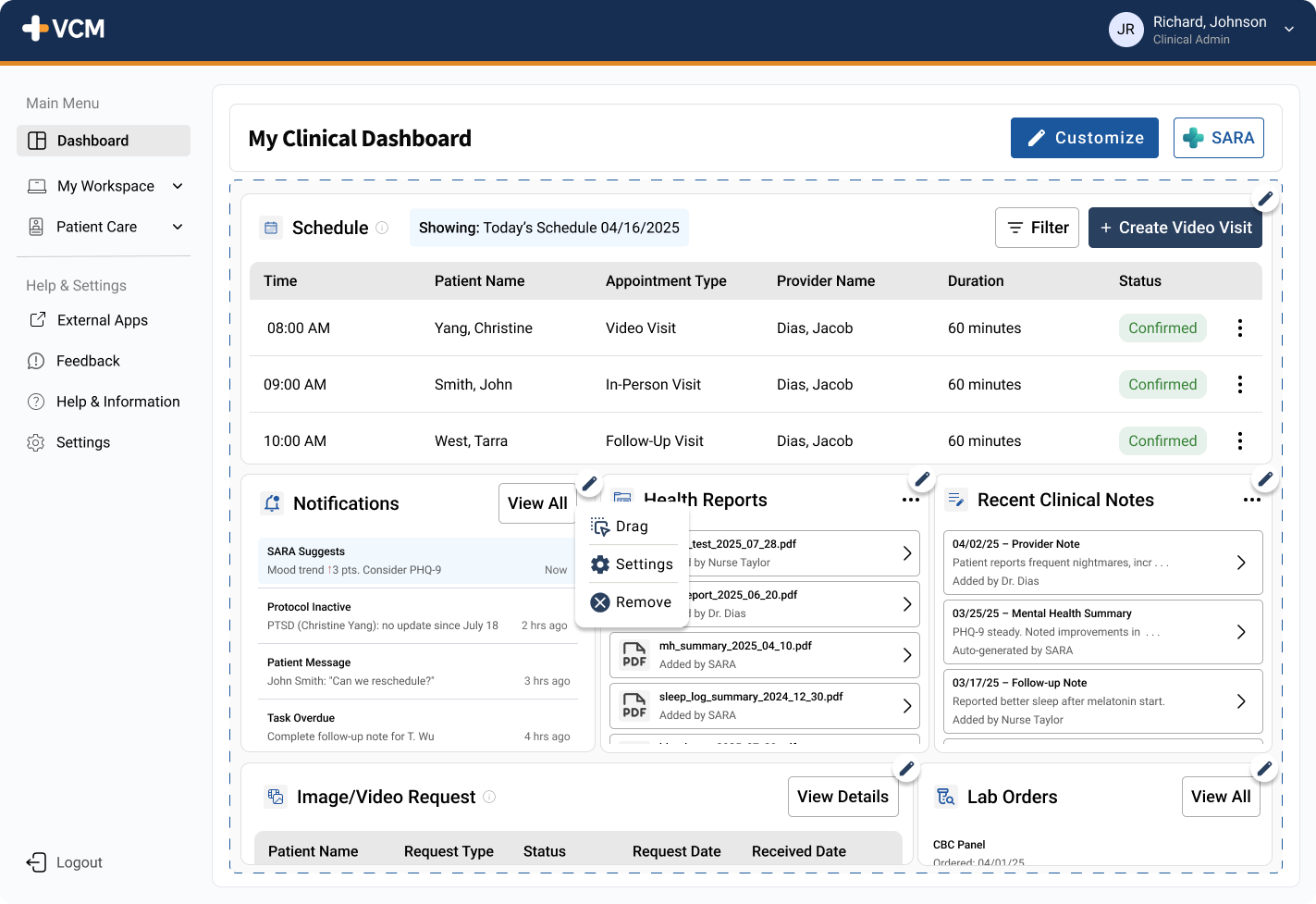
Transition into Customization Mode
Customization mode transforms the dashboard into a personal cockpit: providers drag, drop, and reorder widgets in seconds, creating layouts tailored to their day.
Smart Assistant for Reasoning + Assessment
SARA is a GenAI-powered clinical assistant built on large language models (LLMs). Embedded within the dashboard, it adapts to each provider’s needs, whether that’s summarizing mental health assessments, surfacing critical vitals, or flagging care gaps. Every insight is transparent and traceable, with clear citations to maintain clinician trust. The goal isn’t to replace medical expertise, but to act as a trusted partner, helping clinicians cut through fragmented data so they can spend more time with patients.
Optimizing the Dashboard with SARA
SARA starts working the moment a clinician logs in. It assembles today’s schedule, checks recent assessments, reconciles protocol steps, and surfaces any critical results, ensuring the dashboard is always live and trustworthy. Transparent AI Partner
SARA’s process isn’t hidden. Every step in the sequence is shown, so clinicians see what’s being checked from recent assessments to protocol compliance, building trust in the system.
Contextual Support at the Point of Care
SARA adapts to the clinician’s focus, whether reviewing cardiology vitals, oncology treatment cycles, or chronic disease management. Each conversation evolves naturally, surfacing the most relevant insights in context.
Context-Aware Conversations
SARA isn’t locked to one workflow or specialty. It interprets clinical context and adapts, whether that’s flagging a lab value, checking protocol adherence, or summarizing trends. Each interaction begins with the clinician’s current focus and evolves naturally, just like a real conversation.
Clinical Dashboard Powered by SARA
This is one configuration of the SARA-powered clinical dashboard. Every widget from schedules to lab orders, can be tailored to specialty needs. What you see here is just one example; in practice, each provider shapes their own dashboard.
Key Highlights
At a Glance Patient Context: next appointment, key alerts, and trends.
Protocol Progress Tracker: ensures steps in clinical care aren’t missed.
Open Tasks + SARA Suggestions: combines clinician to dos with AI-powered prompts.
Daily Schedule: anchors the day with upcoming visits.
Configurable Widgets: clinicians can add/reorder widgets like Vitals, Labs, Assessments, or Mental Health Scores.
Outcomes & Impact
Even though the dashboard and SARA are still in early-stage testing, pilot evaluations with clinicians gave us strong signals of value:
Time Savings: Providers reported saving 10–15 minutes per patient on average during prep, primarily from SARA surfacing protocols, labs, and recent notes in one place.
Trend Detection: In a 3-week trial, SARA flagged 6 care gaps (missed PTSD protocol steps, overdue labs, or abnormal vitals) that would have otherwise required manual digging.
Cognitive Load: 82% of pilot participants agreed the dashboard made daily prep feel less overwhelming, reducing reliance on sticky notes and external trackers.
Adoption Signals: 7 out of 10 providers said they would prefer this dashboard over their current workflow if made available in production.
What I Learned
This project taught me several things that I’ll carry into future design work:
Balance Between Flexibility & Focus
Our first iterations leaned heavily on customization, but clinicians quickly felt overwhelmed by too many options. The breakthrough came when we added smart defaults role-sensitive templates that gave providers a clear starting point while still allowing flexibility.Transparency Builds Trust in AI
Early prototypes of SARA were too opaque (“black box” suggestions). By making every AI action visible, citing data sources, explaining reasoning, we reduced skepticism and built confidence.Cross-Specialty Design Requires Abstraction
Primary care, oncology, and mental health providers all wanted different data points, but the interaction patterns(alerts, summaries, tasks) were universal. Designing at the pattern level instead of the data level made the system scalable.Designing for Cognitive Relief
The true value wasn’t in showing more data, but in showing the right data, at the right moment. That reframed our design principles toward clarity, progressive disclosure, and reducing decision fatigue.